Important vascular issues include those of the vertebral artery in the cervical spine. A commonly held belief is that these incidence (-catastrophic or otherwise) are rare with a prevelance of 1 : 100 000. However, the true number may be much greater, as many catastrophic incidents are under - reported due to medico-legal reasons. In my clinical experience, by 2008 I had seen approximately 12 clients with VBI and a further 8 who had petit mal seizures or vaso-vagal syncope with mobilisations to the first rib. The majority of the clients with the 'classic' symptoms of VBI had either a prior incidence from manipulation of the C/S or had a major accident involving the neck - car accidents prior to seat belts, and horse riding incidents were frequently reported. Even a train crash was reported. By 2008 I estimated that I had seen approximately 60 000 clients. Hence, my 20 : 60 000 ratio suggest a 1 in 3000 chance of coming across a client with VBI.
A form of pins & needles in the feet during cycling may be due to claudication. Such claudication may be the result of damage to vessels of the abdominal aortic. Additionally the branches of the abdominal aorta descending into the leg as well as the leg vasculature may be damaged by trauma and/or systemic complications (e.g. Marfan's syndrome, vascular diseases, etc). These problems may be a medical emergency whereby immediate consultation with a vascular surgeon is imperative.
Virchow's Triad in the aetiology of thrombosis may also be of assistence with differential diagnosis. The 3 variables include
-
Changes in vessel wall (endothelial damage)
-
Changes in blood flow (flow volume/stasis)
-
Changes in blood constituents (state of coagulability)
The latter may include screening questions for blood disordes (thrombolytic ones, C-reactive protein , Leiden Factor V, as well as Thalasaemia and Sickle Cell Anaemia), systemic inflammatory conditions (such as Lupus and Scleroderma), the use of oral contraceptives, smoking, diet and frequent flying.
Taylor & Kerry (2005) quote a paper from Sise et al (1989) reporting an average 2 year delay in diagnosis in young people where 93% could have been diagnosed with simple palpation of peripheral pulses.
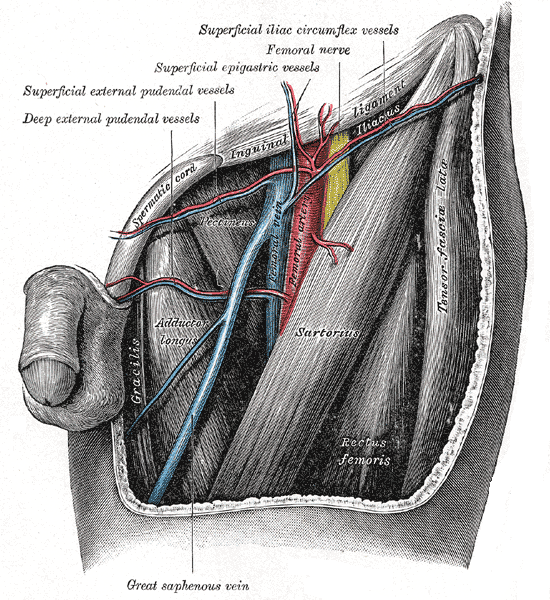 from Gray's Antaomy
from Gray's Antaomy
Vascular complications are potentailly overlooked causes of symptoms. This in part may be due to their relative infrequency compared with other conditions seen by physiotherapists. Futhermore, the symptoms of vascular compromise may mimic those of symptoms arising from musculoskeletal structures. Compromise of a blood vessel to the spinal nerve results in radicular pain. A colleague reported the incidental finding of a family friend's teenage boy whose mother was about to take him to the chiropractor for low back pain. What he noted was the boy had 3 socks on his left foot!!! Immediate examination of the lack of pedal pulses and referal to the A+E department confirmed a diagnosis of spinal artery thrombosis. Unfortunately, most peoples friends aren't astute clinicians that recognise "something which doesn't make sense". Arterial kinking of the external iliac artery during hip flexion whilst cycling (and rowing, skatting and Fjell running) have been known to produce pain affecting the buttock, anterolateral thigh, calf and foot with feelings of paraesthesia and numbness in the toes. Cyclists may also describe the feeling of 'fullness' in the leg and lack of power, cramping and/or ischeamic like fatigue. Although anterior/posterior and lateral compartment syndromes are commonly associated with vascular complications in running, similar type (not necessarily area) of symptoms associated with iliac artery, femoral artery and popliteal artery can be missed during the clinical reasoning process. Generally, symptoms are associated with exertion and external compromise of the blood vessel. Apart from the iliac artery already mentioned other examples include the femoral artery in the adductor canal (b/n the adductor magnus and vastus medialis), and the politeal artery interfacing with the medial head of gastrocnemius. Generally, these conditions are associated with anatomical anomalies whereby the external pressure from repetitive movement gradually damages the external lining of the blood vessel. Besides repetitive microtrauma, any external trauma from an accident needs to consider possible vascular damage or the formation of scar tissue and adhesions which could lead to vascular damage. Other clinical examples, include aortic aneurysm which may be due to valsava type maneuvers. Familial history may also be important in differential diagnosis. Additionally, a history of heavy smoking can lead to internal blood vessel pathology. Similarly, women who take the pill may also be at risk. Aortic stenosis may manifest as a result of arterosclerosis or due to underlying congenital defects. These are screening questions which need to be asked during the subjective examination. During the physical examination, the femoral and pedal pulses should be examined at rest but usually need to be assessed immediately after exercise or in the compromising posture where symptoms normally manifest. Further testing should include ankle blood pressure monitoring of each side. Taylor & Kerry (2005) recommend 20 minutes of rest before testing systolic blood pressure in the left and right brachial artery, posterior tibial and dorsalis pedis and then using the "Ankle to brachial pressure index = Ankle systolic BP / Brachial systolic BP". 1 - 1.2 considered normal, 0.75 - 0.9 indicates moderate disease, 0.5 - 0.75 severe disease and <0.5 is limb threatening. (see: Taylor AJ, Kerry R (2005) Vascular syndromes presenting as pain of spinal origin. Ch 36 in Grieve's Modern Manual Therapy: The Vertebral Column. Ed Boyling JD & Jull GA Elsevier Churchill Livingstone).
The Upper Limb and vascular compromise
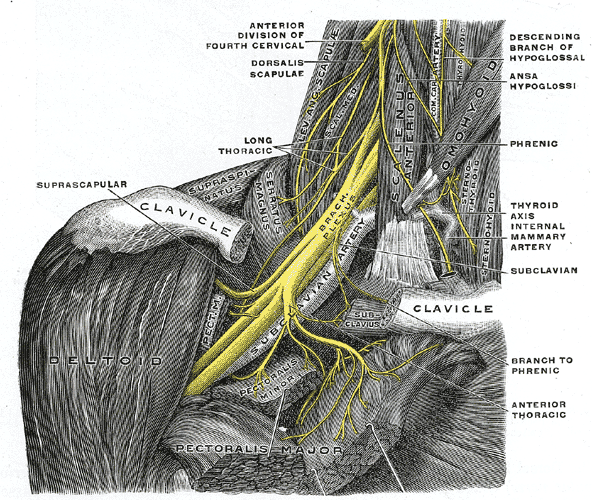
from Grays Anatomy
The posture of the cyclist (and rower) may also make these athletes particularly prone to upper limb and head/neck vascular conditions. Additionally, one of the most common cycling injuries involves landing on the shoulder or outstretched hand resulting in possible neurovascular traction injury, direct trauma and/or clavicular fracture. The latter has been associated with trapezius muscle dysfunction which can be a precipitating variable leading to Thoracic Outlet Syndrome (TOS). Symptoms of TOS can include typical symptoms of neck, shoulder, elbow and hand pain. Occasionally, people describe a sense of swelling (or fullness) in the arm, with/without concommitant pins & needles or numbness. Vascular components of TOS may be less prevelant than neurological ones. Yet this may be due to mis-diagnosis as the plethora of tests (Adson's, Allen's Halstead's manoeuver, Roos's EAST test) may be falsely positive or negative and variable b/n examiners. Hence, the examination must use the multitude of variables at the clinicians disposal, both Subjective symptoms & Physical signs - inductive and deductive reasoning, to make sense of the clincal picture. When in doubt and further investigations are required, by using the weight of probability from many variables, it may also make the argument for further testing more convincing to a medical colleague.
Paget - Schroetter syndrome is a deep venous thrombosis of the subclavian - axillary venous system, also known as "effort thrombosis" (Rutherford 1998, Zell et al 2001) and may account for about 3-7% of all DVT's (Taylor & Kerry 2005). The average patient is in their late 20's to early 30's and males present 3 times more commonly than females. Most commonly complain of quick insidious arm pain (70% in dominant arm), with possible supraclavicular fossa and ipsilateral neck pain. Most commonly occurs in activity with repetitve upper arm, over shoulder height, movements. The usual aetiology is Virchow's Triad which means that specific screening questioning is required. Additionally, other risk factors may include thoracic outlet factors such as cervical rib, anomalous first rib, hypertrophy of the anterior scalene, subclavius or pectoralis minor as well as endogenous factors such as activated protein C resistance and anticardiolipin antibodies (Ellis 2000 in Taylor & Kerry 2005).
Taylor & Kerry suggest that observable signs of vascular compromise may include skin pallor or cyanosis - both resting and positional, swelling, and/or superficial venous dilation. Corneal arcus or xanthelasmas (yellowish raises skin changes) around both eyes may be associated with hyperlipidaemia and hypercholesterolaemia. Staining of fingers may be a more accurate indicator of tobacco consumption. Obesity and state of mental awareness may also reflect underlying cerebrovascular state.
Hand and digital examination should also include nail squeezing - indicative of capillary refilling time. These should be perfomed in various positions of potential vascular compromise. Nail abnormalities may be present. Pulses should be tested, stethescope auscultation should be undertaken and the pressure cuff sphygmomanometer and hand held doppler or automatic blood pressure monitor used (Taylor & Kerry 2005).
Taylor & Kerry (2005) argue quite strongly that vascular examination is such a miniscule part of both under-graduate and post-graduate degrees that we may be implicated in delayed diagnosis and initiating innapropriate treatment.
Clinical example : Facial Numbness
Blood Disorders
Thalassemia (British English: thalassaemia) are forms of inherited autosomal recessive blood disorders that originated in the Mediterranean region. In thalassemia, the disease is caused by the weakening and destruction of red blood cells. Thalassemia is caused by variant or missing genes that affect how the body makes hemoglobin. Hemoglobin is the protein in red blood cells that carries oxygen. People with thalassemia make less hemoglobin and fewer circulating red blood cells than normal, which results in mild or severe anemia.
Thalassemia can cause significant complications, including pneumonia, iron overload, bone deformities and cardiovascular illness. However this same inherited disease of red blood cells may confer a degree of protection against malaria, which is or was prevalent in the regions where the trait is common. This selective survival advantage on carriers (known as heterozygous advantage) may be responsible for perpetuating the mutation in populations. In that respect, the various thalassemias resemble another genetic disorder affecting hemoglobin, sickle-cell disease.
Factor V Leiden, also known as Leiden Factor 5 (and sometimes factor VLeiden) is the name given to a variant of human factor V that causes a hypercoagulability disorder. In this disorder, the Leiden variant of factor V cannot be inactivated by activated protein C. Factor V Leiden is the most common hereditary hypercoagulability disorder amongst Eurasians
Uploaded : 17 November 2017




